BY BECCA PAVA
When I was 19, I had another bad flare up of gastroparesis, a digestive disorder which causes paralysis of the stomach. My flare up was complete with incessant vomiting, inability to eat any food or keep down any liquid, and terrible cramping pains and constipation and bloating. My mom and my adolescent medicine doctor confronted me and insisted that I be admitted to either a psychiatric unit or an eating disorder facility. They assumed that if the typical treatment for gastroparesis wasn’t working, there must be more to it than just gastroparesis. My GI doctor figured I had a lot of psych issues going on along with the gastroparesis so maybe if we cleared up the psych issues I would be easier to treat. He didn’t specialize in gastroparesis and had told us he had never seen a case as bad as mine before.
“I’ll go to the eating disorder facility if I have no other choice,” I told them, figuring it had to be less crazy then another psychiatric unit filled with catatonic, manic, or aggressive characters; and nurses that felt the need to treat all the patients like toddlers or even bad dogs that needed constant disciplining. I had been in many psychiatric units for my schizoaffective disorder that was now under control, but I was feeling angry and like everyone had given up on me getting better.
“I have gastroparesis, not an eating disorder,” I told them a million times in protest.
“People with gastroparesis can still eat a modified diet and get enough nutrition in,” the doctors insisted along with my mom. At that point in my life, I hadn’t joined any support groups or done enough research to know that some people with gastroparesis not only can’t eat anything but also can’t even manage sips of water or even tube feeding. Those people actually have to depend on intravenous means of nutrition called TPN despite treatment with diet changes, meds, and gastric pacemakers. I also didn’t know back then that I was one of many with gastroparesis who were labeled as having an eating disorder, when the truth was the problem actually was a paralyzed stomach (gastroparesis).
I had run out of options when my parents threatened to kick me out of the house if I didn’t go to the eating disorder unit, so I drove up to Boston with my mom and was admitted to the Behavioral Care Center’s eating disorder unit. The Behavioral Care Center was located on the third floor of a large health complex. One half of the Behavioral Care Center was the eating disorder treatment unit, and the other half was a psychiatric unit. They both had locked doors, but the intake for the eating disorder unit occurred on the first floor and included being stuck for ten tubes of blood to test for tons of nutrition deficiencies so they knew what vitamins you needed.
Then I had to meet with a social worker, a nurse, and a doctor. Once the lengthy intake interviews in the office area were completed, the interviewer took my suitcase and walked my mom and me up to the unit. A wave of dizziness washed over me as I stood up to follow her to the doors.
“You have to say good bye to your mom here,” she told me. “She can’t come onto the unit with you.”
“Can’t she help me unpack and settle in?” I asked.
“No, that‘s against unit rules, she can come back for visiting hours tomorrow at 6 to 8 PM.” She told us.
“But we live almost two hours away, she can’t come back for a few days,” I explained.
“Can I just walk onto the unit with her?” my mom asked.
“No, it’s against policy,” the thin lipped woman with the tight ponytail, told my mom.
“So I can’t even walk her in to say good bye?” my mom asked incredulously.
“You can say goodbye here.”
“I love you,” my mom told me, “It’s ok, I’ll be back as soon as possible.”
I hugged my mom so tightly I could smell the comforting scent of her “Powder Fresh” Dove deodorant. She hugged me back just as tightly and rubbed my back gently.
“Rules are rules,’’ the interviewer said.
The eating disorder unit was full of rules too. I remember that I learned them quickly in my first few days there. No clothes with pockets ior shirts with hoods in the dining room. No discussions of food or calories or nutrition facts. No pacing the halls. Absolutely no exercise. No using the bathroom within an hour after meals and within half an hour after snacks. Always fill out your food diary cards after all meals and snacks. Go to all your groups. Don’t go to your rooms during free time unless you earned a green bracelet. You have to eat 100% of meals and snacks, or you have to stay after meals to drink Boost. You have to stay for the full fifteen minutes after meals or snacks even if you don’t drink the Boost. You have exactly one hour to eat meals and half an hour to eat snacks. The list goes on and on, and they enforced the rules like drill sergeants.
After my mom left, I couldn’t help it, I started to bawl. I felt like a five-year-old that had just been abandoned in an alien place.
“Don’t cry. Stop crying, there’s nothing to cry about, you’re nineteen aren’t you? Not two!” the woman told me.
“I’m sorry,” I sobbed, crying even harder. One of my famous burning, cramping pains shot through my stomach.
The woman buzzed me through the locked doors and handed me off to a nurse.
“Hi, I’m Jackie,” the nurse greeted me. “It’s okay, you’ll be okay. I’ll get one of the techs to help you go through your suitcase and put your things away.”
“Thanks,” I told her, still crying so hard that I felt like I might throw up.
A tech named Matt brought me to my room. It was large, and had two simple wooden framed beds with hospital issue white sheets and blue blankets. Each side of the room had its own wooden night stand and dresser that were nailed to the floor with metal plates. My side of the room was near the large window. The other bed was near the door and the bathroom and double spaced closet. A lonely IV pole with what I immediately recognized as a Kangaroo brand feeding pump stood guard by the other bed.
“You’re sharing a room with a girl named Brittany. She’s twenty; you’ll like her alot,” he told me.
“Where is she?” I asked.
“She’s at group. We have therapy groups all day here; art therapy, talk therapy, DBT therapy which is a type of talk therapy that uses mindfulness, emotion regulating skills and skills meant to get you through crisis called ‘distress tolerance skills’ to deal with self destructive behavior patterns, yoga, all sorts of groups. We keep you guys busy.” Matt answered. “Now let’s get to your suitcase.”
Matt pulled on some gloves which made me feel like he thought I was contaminated or something, and then he thumbed through each article of clothing, turning them inside out, shaking them and everything. He got to a pair of sweatpants with a drawstring waist.
“Do you need this drawstring?” he asked me.
“Yeah, the pants won’t stay up without them,” I told him.
“Well we’ll have to set the pants aside then, and send them home with your mom next time she comes because the drawstring is considered a safety risk on this unit.”
“Oh ok,” I told him feeling annoyed. I wasn’t crazy, I didn’t even actually have an eating disorder, and yet I was being treated like a mental patient. Anger course through my veins.
We hit another road bump when we get to my precious teddy that I made at Build-a-Bear workshop that I sleep with every night along with my baby blanket from childhood.
“We don’t allow any stuffed animals or bedding from home. You’ll have to send these home as well,” he told me.
“But I can’t sleep without them.” I pleaded.
“It’s against unit policy,” he told me.
“Why?” I asked
““It’s just the rules, that’s all. I think we had bed bugs brought in at some point or something so now we don’t allow it,” he attempted to explain.
“These don’t have bed bugs, I promise,” I said. “I need those; I’ve slept with them every night forever.
“It’s against the rules, I’m sorry”.
After I had been violated by a clothing search, and had my precious Teddy and Blankie confiscated, I tried to use the bathroom and found that the door was locked. I went up to the nurses’ station and was told by the nurse that all the bathrooms in the rooms were locked and I would have to get my assigned tech to open it and then show him the contents of the toilet before I flushed. Eww! This was getting worse and worse.
At dinner, Jackie the nurse came up to me and asked if I wanted peanut butter and jelly, cheese, or tuna or turkey as a sandwich for dinner.
“I can’t eat any of those, I’m way too nauseous, it would make me sick,” I told her.
“Well I have to order you something. Tonight is a free pass for you because it’s your first meal here. You won’t have to stay afterward for a Boost if you don’t eat 100%, but starting tomorrow the dietitian will order you a diet and you will have to follow protocol. What can I order you for tonight?”
“Peanut butter and jelly,” I told her.
When the meal came up I took one bite of the sandwich and then felt it sink down my throat in a lump. My stomach retaliated by churning and swirling around and forcing it back up into my throat. I felt it rise up and swallowed it down quite a few times. I sat there the rest of the hour ignoring the food and whole milk that had been placed in front of me as pain jackknifed through my belly.
Back in my room that night I introduced myself to Brittany, a tall rail thin girl with long silky jet black hair, blue eyes, and a feeding tube delicately threaded up her nose down into her stomach.
“I’ve been here two weeks, and have had the tube since the second day here,” she told me.
That worried me, would they give me a feeding tube?
“Why did they put it in?” I asked her as gently as possible.
“Because they said I was too underweight and I wasn’t eating 100% or drinking my Boosts,” she explained.
Now I was really worried. I slept fitfully that night with a balled up sweatshirt in my arms as a weak replacement for my beloved teddy and blankie.
At 6:15 AM, I was awakened by a Russian man with a soft smile, fuzzy beard, and a thick accent.
“Stay lying down, I need to take your blood pressure,” he told me, needing to repeat himself twice before I understood what he was trying to say. He took my blood pressure and then told me to stand up. I stood up and he took my blood pressure again. I glanced at the readout on the automatic machine. 85/52, not a good blood pressure considering normal is 120/80. With all my knowledge from my hospitalizations and doctors’ appointments I knew that meant I was dehydrated and I wasn’t surprised. I hadn’t been able to keep down anything more than sips of water or Gatorade for almost two weeks.
The Russian man wrote down the blood pressures on a clipboard and then handed me a thin hospital gown.
“Take everything off, even your underwear and watch and those bracelets and change into this. You can keep this gown, every morning you will change into the hospital gown and go down the hall with me to get weighed on the scale in the dining room. Understand?”
I nodded and took the gown. The Russian man opened the bathroom door for me and I changed and followed him down the hall feeling very open and vulnerable with my bare bottom barely covered by the worn down hospital gown wrapped tightly around my body and clutched for dear life in my fist to prevent it from blowing open in the hallway’s breeze.
The scale in the dining room was a flat black surface with a wire attached to it leading to the LED display on a dining room table where a nurse was sitting with her own clipboard. As I stepped up onto the scale she tipped the display toward her so that there was absolutely no way I would see the readout of my weight.
After I stepped off the scale the Russian man gestured for me to stay there for a minute and he went up to the nurse and showed her his clipboard.
“Becca, I want you to go back to your room and drink some Gatorade. Your blood pressure drops too low when you stand up. I also don’t want you to get out of bed until the doctor evaluates you further. Okay?
“Okay, but I don’t know how much Gatorade I can drink, I get really nauseous.”
“Well you have to try. Take little sips slowly. Vlad will walk you back.”
The Russian man, Vlad, walked me back to my room, left, and then returned with a bottle of blue Glacier Freeze Gatorade and a cup of ice.
Okay, I can do this, I tried to pep talk myself as I poured the Gatorade over ice, I took a sip and immediately felt nauseous. I took another sip and felt my stomach churning in protest. The Gatorade rose back up in the back of my throat, I swallowed it back down along with the bitter and sour bile that had risen up with it. My stomach suddenly felt as full as though I had just finished Thanksgiving dinner. I pushed the Gatorade away from me and fought back tears.
As I lay back in defeat, Brittany was getting her shower stuff ready.
“The only time we can take showers is in the morning between 7 and 8:15 AM. The showers are locked the rest of the day because they’re afraid we’ll use the showers to purge,” Brittany explained. “Only four people can shower at a time so there’s a shower list to sign up on.”
I groaned, since I was stuck in bed until the doctor cleared me, I was going to miss my shower for the day. If I hadn’t been contaminated when the tech pulled on gloves to go through my belongings, I was certainly going to be a dirty, sweaty mess soon.
The nurse came in with my meds at 8:45. By that time I had been unsuccessfully trying to distract and entertain myself for the past two hours. I had tried to read, tried to journal, tried to knit, and even tried to go back to sleep, but I was too nauseous to sleep and too uncomfortable and nervous to do anything else.
“You didn’t drink your Gatorade,” the nurse said, first thing when she came in the room. She had shoulder length brown hair but no smile lines.
“I tried really hard, but it made me way too nauseous,” I explained.
“Well you need to drink it. Your admission labs came back and they were a mess. You’re both very malnourished and very dehydrated. You need to be eating and drinking or we’re going to have to send you out to the hospital.”
“I hate hospitals,” I told her.
“Well you’re going to need IV fluids if you can’t drink the Gatorade.”
“I’ll try to drink some with my meds,” I told her.
“Okay, well Dr. Melrose is going to come evaluate you this morning and the dietitian will see you too. Until Dr. Melrose clears you, you are on strict bedrest. I brought you a bell to ring. If you need to go to the bathroom just ring it and one of the techs will help you there.” The nurse handed me an old fashioned bell to ring and then handed me a little plastic cup filled with my cornucopia of meds.
I swallowed the colorful pills and capsules with two small sips of Gatorade and then swallowed back down five more times to swallow all the Gatorade and bile that kept rising back up in my throat. Now I felt like I had eaten Thanksgiving dinner and then binged on a pint of ice cream. My stomach was distended and I felt squeezing pains.
“You need to drink more than that,” the nurse chastised me.
“I can’t, I’m way too nauseous, I’m on the verge of throwing up.”
“You need to try.”
“I can’t do anymore, I really can’t. I’ll throw up the meds.”
“The amount of Gatorade you drank shouldn’t make you vomit.”
“Well I almost did, I have gastroparesis, I really can’t do anymore.” I said.
“Well you have to try harder or go to the hospital. Dr. Melrose should be in to see you before noon.”
“I have to just stay in bed until then?” I asked
“She may be here sooner. Or the dietitian. I don’t know.”
“But I have nothing to do,” I protested.
“Yes you do, you can work on drinking Gatorade and your breakfast will be here soon.” With that she took back the empty med cup and left the room
The dietitian came in first. Her name was Elizabeth. She explained to me that I needed 1400 calories a day to start off with, and that the diet here consisted of three meals and three snacks.
“I have gastroparesis,” I explained to her.
“It’s good for gastroparesis to have meals and snacks as opposed to just three large meals a day, so we’ll design a meal plan that fits your needs,” she assured me and laid out exactly how many proteins, carbs, fruits, veggies, dairy, and fats I would need a day. She promised me that they could accommodate my vegetarian diet as well. Then she asked me how long it’s been since I’ve eaten.
“It’s been close to three weeks,” I admitted. “I’ve just felt so nauseous and full all of the time.”
“Have you ever had an NG tube?” she asked me.
My whole body tightened. I knew I had to tell her the truth but I was terrified of what she would do with it, and why she needed that information.
“I’ve had them in the past,” I said slowly.
“Do you think you need one now? To help you start getting used to nutrition again?”
I was about to immediately answer no, that was my gut reaction, but then I thought about my health. The last time I had been weighed and actually seen the readout I was 86 pounds, way too low for my 5’0 frame and I knew it. Plus the latest bloodwork showed severe malnutrition and dehydration. If they put in an NG I might start feeling better and get acclimated to getting food into me at a very slow rate. I knew that once I hit this point with my gastroparesis I would vomit everything up, but if they started a tube feed at 5 ml and hour and slowly titrated it up 5 ml an hour at a time, I might not vomit and my stomach might get used to having food in it.
“Maybe,” I told her. “Do you have really thin tubes?” NG tubes can be extremely uncomfortable, especially when they first go in. For me NG tube insertions can be excruciatingly painful.
“We do, we have pediatric sized tubes.”
“Okay, whatever you think then.”
“I’ll see what Dr. Melrose and the team think,” Elizabeth said.
Dr. Melrose showed up an hour after Elizabeth left.
“You’re very malnourished and dehydrated. I spoke with Elizabeth and we’re going to give you one day to try to eat and drink on your own. If you can’t drink Gatorade or eat at least 50% of your meals and snacks then we’ll have to put in an NG tube for feeding and hydration.”
She talked to me a while longer about both my medical and psychiatric history. I explained to her that I have had gastroparesis since I was ten and that in addition to the gastroparesis, I had an eating disorder from age twelve until age fifteen, but that I am no longer anorexic and have never been bulimic. I let her know that I would like to weigh 100 pounds and she agreed that was a good starting goal weight. I also let her know my history of anxiety, depression, and hearing voices that no one else could hear.
“That must have been rough. I’d like to put you on a medication called Compazine,” Dr. Melrose told me. “I’ll have you take it every six hours, it’s an anti-nausea medication that will hopefully help you to be able to keep down food and drinks. Do you want to try it?”
“Sure, I’m desperate.”
The first Compazine was due half an hour before lunch. I swallowed it with a sip of Gatorade and then still had to swallow back vomit multiple times in the next fifteen minutes. Unfortunately for me the pill didn’t kick in in time for lunch and I managed no more than a spoonful of applesauce and a half a sip of Boost. The nurse just clicked her tongue, scolded me for not trying hard enough and took the food and then the Boost away.
The nausea seemed to lessen slightly a couple hours after lunch but I still felt so stuffed that I was worried I would bust open. Dinner didn’t go much better than lunch because of the intense feelings of fullness.
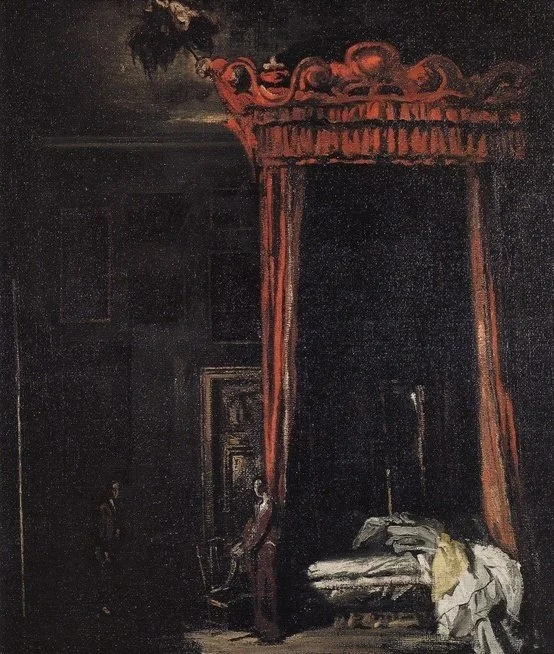
Related: Vampira, The Witch That Took Down This Hollywood Legend
The following day when Dr. Melrose came by I already knew what she was going to say so I was not surprised when she came in with a length of tubing, gloves, lubricant, and tape, all on a sterile metal cart.
“Well since you weren’t able to eat or drink enough on your own, we’ll have to help you out a little with the feeding tube.” Dr. Melrose explained.
“I’m nervous about this; they hurt so badly going in.” I felt my body tightening with anxiety.
“Just relax, I put these in all the time. I’ll be really gentle.”
“Ok,” my voice shook.
Dr. Melrose slid her gloves on and pulled the NG tubing out of the packaging. She held it up to my face, along my cheek, and measured it down to my stomach, then marked her measurement with a black sharpie. When she started dipping the tube in lubricant, I could smell it and the scent caused sensory memories so strong that I could already feel the gagging sensation in the back of my throat and pressure against my nose.
“It’s okay, it’s a very thin pediatric tube, and like I said, I’ll be gentle,” Dr. Melrose had caught the expression on my face.
She raised the tube to my face.
“I’m going to insert it into your nostril now. You’re going to feel a little pressure. When I tell you to swallow, swallow hard over and over again until I tell you that you can stop.”
“Okay.”
The tube entered my nose and the lubricant scent was overwhelming. It was all I could smell and taste, and even think about. The pressure intensified as she slid the tube higher up. She hit resistance. I felt sharp intense shooting pains as she forced the tube past the resistance. Tears began rolling down my face, first just oozing out, then down-pouring as the pain reached an excruciating level.
“Stop, I can’t take it!” I cried.
Dr. Melrose stopped.
“I’m hitting some resistance, but I’m almost past it, I just need to twist the tube a little. You should be more comfortable in a sec. Can you give me a few more seconds?”
“I guess…”
“Ok, good.”
I felt the tube piercing through what felt like a wall of cartilage. I could swear there was a popping sound and sensation and then I felt myself gagging on the tip of the tube coming down the back of my throat.
“Okay, great, now swallow, swallow, swallow.”
I swallowed hard and just kept swallowing as the tube continued to completely gag me as it shoved its way down my throat, esophagus, and into my stomach.
“All right, I think I’m in!” Dr. Melrose finally announced, “you can stop swallowing. I’m just going to check placement.”
The doctor hooked up a syringe with air in it to the end of the tube and put her stethoscope over my stomach. She injected the air into my stomach and listened with the stethoscope to see if she could hear it enter my stomach.
“Its right in there, now,” she smiled at me. “So we’re going to run Gatorade into your tube during the day, and we’ll run a tube feed called Nutren 1.5 in at night. We’ll start at a really low rate and slowly increase it until we get to a goal rate that you can tolerate.”
“Thank you so much,” I smiled at her. The smile felt so foreign on my face after all of the crying and misery I had been going through for the last three weeks. The tube was ugly looking, my throat was scratchy and sore, and I felt like I was gagging every time I tried to swallow, but now I had a way of getting desperately needed nutrition and hydration and that gave me some relief.
At least now I had a band aid. A temporary solution. That was all life ever offered me in those days.